

Explore the synergistic sedative effects of CNS depressants and how they interact to enhance therapeutic outcomes and risks.
The central nervous system (CNS) depressants are a class of medications that act to reduce brain activity, leading to effects such as relaxation, sedation, and, in some cases, sleep. When used alone, these drugs can help manage conditions like anxiety, insomnia, and muscle spasms. However, the combination of multiple CNS depressants—either intentionally prescribed by healthcare providers or accidentally consumed—can lead to synergistic sedative effects that significantly amplify the overall impact on the body.
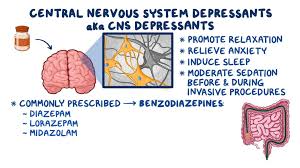
CNS depressants include a variety of substances such as benzodiazepines, barbiturates, opioids, alcohol, and certain muscle relaxants. Each of these works by depressing the central nervous system through different mechanisms, but their combined effects on the body can be potent and sometimes dangerous.
Benzodiazepines, for example, increase the effect of a neurotransmitter called gamma-aminobutyric acid (GABA). This neurotransmitter inhibits brain activity, leading to sedative and calming effects. Medications like diazepam, lorazepam, and alprazolam are commonly prescribed for anxiety and sleep disorders. Barbiturates, another class of CNS depressants, work in a similar way by enhancing GABA’s activity, though they are more potent and carry a higher risk of overdose compared to benzodiazepines. These are often used for anesthesia and in the treatment of epilepsy, but they too can cause significant sedation when combined with other CNS depressants.
Opioids, such as morphine, oxycodone, and hydrocodone, target the opioid receptors in the brain to alleviate pain. They too contribute to CNS depression by slowing down brain function and reducing the perception of pain. When mixed with other CNS depressants, the cumulative sedative effect can be life-threatening. Opioids suppress breathing and heart rate, and when taken with alcohol or benzodiazepines, these vital functions can become dangerously depressed, leading to respiratory failure or coma.
Alcohol is one of the most commonly abused CNS depressants. As a central nervous system depressant, alcohol slows down brain activity, impairing coordination, judgment, and motor skills. It also increases the effects of GABA and inhibits the release of other neurotransmitters like glutamate, which further contributes to the sedative effect. When consumed with other CNS depressants, alcohol can magnify the risks of sedation, dizziness, and unconsciousness. This is why mixing alcohol with prescription sedatives or painkillers is strongly discouraged.
When two or more CNS depressants are used together, the combined effects can lead to synergistic sedation, where the overall sedative effect is greater than the sum of individual effects. For example, combining a benzodiazepine with an opioid can significantly enhance the sedative properties of both drugs. The user may experience profound drowsiness, confusion, difficulty breathing, or loss of consciousness, all of which can be potentially fatal.
The dangers of this synergistic sedation are particularly concerning in cases of unintentional misuse or recreational drug use. Many people may not be fully aware of how potent the combination of these substances can be, especially if they are mixing medications prescribed by different doctors or combining them with alcohol. For instance, a person may take an opioid for pain and then use a benzodiazepine prescribed for anxiety, unknowingly increasing their risk of overdose.
Healthcare providers are well aware of the risks of synergistic CNS depression and often take great care to avoid prescribing these substances together. In cases where it is medically necessary to combine CNS depressants, doctors carefully monitor the patient’s condition and may adjust doses to minimize the risk of dangerous interactions. Additionally, they provide guidelines on proper usage, making it crucial for patients to follow the prescribed regimen and communicate openly about other medications or substances they may be taking.
In conclusion, while CNS depressants can be beneficial for treating various medical conditions, their synergistic sedative effects pose significant risks when used in combination. The enhanced depressant effect can lead to respiratory depression, unconsciousness, and even death. It is essential for both patients and healthcare providers to be mindful of the risks associated with combining these drugs and to take preventive measures to ensure safety.
