
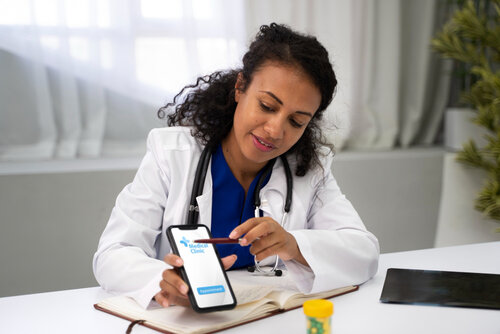
Integrating Ambient Intelligence with EHRs
Integrating ambient intelligence with EHRs and clinical workflows isn’t just a tech upgrade—it’s a paradigm shift.






© 2024 Crivva - Business Promotion. All rights reserved.