

Gum disease is inflammation of tissues and bone supporting teeth……
How the Condition Develops
Dental plaque forms quickly after meals and hardens into tartar if not removed. This buildup irritates gum tissue, causing redness, swelling & bleeding. In early stages, the problem is limited to soft tissues and is reversible with timely care. If bacteria extend below the gumline, supporting bone is affected, pockets deepen & teeth can loosen. Understanding this sequence is useful because every step in management aims to interrupt the biofilm cycle and reduce inflammation before long-term damage occurs.
Early Signs That Need Attention
Bleeding during brushing or flossing, persistent bad breath and gum tenderness are common early warnings. Receding tissue, tooth sensitivity to cold & subtle spacing changes may follow as support is lost. Pain is not a reliable signal; many cases progress quietly. Checking gums in a mirror for color changes along the margins, tracking occasional bleeding and noting any sour taste from one area help you recognize trouble early & seek care before intervention becomes complex. Improve your gum health with periodontal dentistry in Campbelltown! Book your consultation today through our website.
Examination That Sets the Course
A structured periodontal exam measures pocket depths, records bleeding sites and reviews radiographs to assess bone support. The clinician evaluates bite forces, existing restorations & signs of grinding that concentrate stress on specific teeth. Medical history and medications are reviewed because dry mouth, diabetes and hormonal shifts influence outcomes. This information becomes a baseline to judge progress, decide between non-surgical or surgical steps & assign appropriate maintenance intervals once active therapy is complete.
First-Line Therapy: Scaling and Root Planing
Non-surgical cleaning above and below the gumline removes soft plaque & hardened tartar. Local anesthesia improves comfort while hand instruments and ultrasonics reach deep contours. Smoothing root surfaces reduces bacterial retention & allows tissue to reattach, often shrinking pocket depths by one to two millimeters when home care is consistent. Treating the mouth in a short window limits reinfection between visits. After several weeks, a re-evaluation confirms healing and identifies sites that still require attention.
Adjunctive Antimicrobial Strategies
Bacteria repopulate quickly, so targeted antimicrobials can support mechanical cleaning. Short courses of systemic antibiotics may be reserved for acute infections or specific aggressive patterns. More commonly, localized medications-chips, gels or microspheres-are placed in deep pockets after debridement to deliver therapy where brushes cannot reach. Antiseptic rinses can help reduce bacterial counts, but they work best as additions to thorough cleaning rather than replacements. The goal is to suppress pathogens while tissue heals and habits improve.
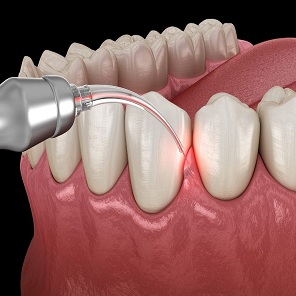
Surgical Options for Residual Pockets
When pockets remain deep or bone defects persist after non-surgical care, surgical access improves visibility & completeness of cleaning. Flap procedures allow removal of residual tartar and reshaping of irregular bony edges that trap plaque. Regenerative techniques-guided membranes, bone graft materials or biologic mediators-are considered for specific defect shapes to rebuild lost support. Soft-tissue grafts treat recession, protect roots from sensitivity & resist future breakdown. Choice depends on defect anatomy, habits and overall health.
Daily Brushing That Targets the Margin
Home care determines whether professional gains last. Brush twice daily for two minutes with a soft manual or powered brush. Angle bristles at about 45 degrees toward the gumline, use short strokes and cover every surface systematically. Apply light pressure to avoid recession. Replace brush heads every three months or sooner if bristles splay. A powered brush helps users with limited dexterity or inconsistent technique. Keeping the routine simple & repeatable is better than complex steps that fade.
Interdental Cleaning That Actually Fits
Most breakdown begins between teeth, so a daily method for those spaces is essential. Floss is effective when contacts are tight & technique is sound. Where gaps are wider, interdental brushes sized to slip without force remove more plaque. A water flosser helps around bridges, implants and orthodontic appliances. Ask for sizing guidance so tools fit without traumatizing tissue. Pick one method you will perform nightly & add others only if you can sustain them comfortably over time.
Food Choices and Tobacco Control
Balanced meals with adequate protein, vitamin C, vitamin D & calcium support repair. Limit frequent snacking on sticky carbohydrates and acidic drinks that fuel bacteria and soften enamel. Drinking water after snacks helps clear debris. Tobacco is the strongest modifiable risk factor; quitting improves healing, reduces pocket depths & lowers tooth loss. Nicotine replacement, medication and counseling increase success. Alcohol in excess dries the mouth & impairs sleep, both of which can worsen inflammation.
Medical Conditions That Change the Plan
Diabetes, pregnancy, autoimmune disorders and medications that reduce saliva or enlarge gums alter risk & response to care. Better glucose control reduces infection, improves outcomes and lowers surgical needs. During pregnancy, more frequent cleanings and meticulous home care manage heightened tissue responses; the second trimester is a common window for non-urgent procedures. Share full medication lists & health updates so the dental plan can be coordinated with medical care and adjusted as conditions evolve.
Implants, Aligners and Restorations
Implants can develop mucosal inflammation and bone loss when plaque accumulates. Specialized instruments & gentle techniques protect implant surfaces during maintenance. For aligners and fixed orthodontic appliances, biofilm builds around attachments and under trays; interdental brushes & water flossers become crucial. Crowns and bridges require threaders or small brushes to reach margins and pontic areas. Asking for tailored instructions for each device or restoration prevents missed sites that commonly trigger recurring problems.
Maintenance Visits That Lock In Results
After active therapy, maintenance every three to four months interrupts biofilm before it hardens and allows pocket monitoring. These visits include site-specific cleaning, reinforcement of technique & revisions when crowding, restorations or life changes alter risk. Stable pocket depths, minimal bleeding and smooth root surfaces are the success markers. If bleeding returns or depths increase, escalate care promptly rather than extending intervals. Viewing maintenance as part of treatment-not an optional extra-protects the investment you already made.
Warning Signs That Call for Prompt Care
Ongoing bleeding, gum tenderness, persistent bad breath, a bad taste from one area, newly shifting teeth or sensitivity from exposed roots are red flags. Sudden swelling or a pimple-like bump on the gum may indicate an abscess that needs urgent attention. Clenching & grinding can worsen mobility and should be managed with bite adjustments or protective splints. Do not wait for pain; deterioration often advances quietly. Early visits simplify solutions and limit the need for surgery.
A Practical Plan You Can Start Today
Schedule a comprehensive exam with charting & radiographs, then complete recommended non-surgical cleaning in a tight timeframe. Commit to one nightly inter dental method and a consistent two-minute brush routine. Add an antiseptic rinse after mechanical cleaning if advised. Stop tobacco use with a structured program. Return for maintenance every three to four months and shorten intervals if bleeding persists. For sites that remain deep, consider localized antimicrobials or surgical correction rather than repeating the same steps without change.
What Improvement Looks Like Over Time
Within weeks of thorough cleaning & steady home care, bleeding decreases and tissue firmness improves. Over months, pocket depths shrink as inflammation resolves and attachment tightens. Breath becomes fresher, chewing feels more comfortable & professional cleanings take less time. Long-term success means keeping natural teeth functional with the least invasive care possible. Consistent daily habits, targeted professional support and timely adjustments produce stable outcomes that hold up across life changes, restorations and dietary shifts.
Key Takeaways for Lasting Stability
Mechanical plaque control is the foundation, adjuncts support healing & maintenance protects results. Nutrition and tobacco control influence every step. Medical conditions and dental devices require tailored strategies. Track early signs, respond quickly & keep intervals short until tissues remain stable. With this approach, most cases can be controlled predictably, reducing the need for extensive procedures and preserving comfortable function over the long term.
About Bio.
Ansley has 12 years of experience in the dental world. You can find his thoughts at childrens dentistry blog.
